Stress, often underestimated as a mere psychological burden, has profound systemic effects—and among the most serious is its potential link to stroke. While the relationship between chronic stress and cardiovascular disease has long been recognized, emerging research underscores that emotional, psychological, and physiological stressors may significantly elevate the risk of both ischemic and hemorrhagic strokes.
At Wyckoff Heights Medical Center, we are dedicated to stroke prevention through comprehensive, evidence-based care and patient education. Current findings suggest that chronic stress contributes to cerebrovascular risk via multiple mechanisms, including dysregulation of blood pressure, heightened inflammatory responses, and endothelial dysfunction. As a trusted community hospital with a specialized stroke team and advanced diagnostic technology, Wyckoff offers the clinical expertise necessary to evaluate, manage, and reduce your risk.
Understanding how stress influences the vascular system is crucial—not only for individuals with underlying health conditions, but for anyone coping with sustained psychological or physical stress. Early recognition and intervention can make a significant difference.
How Can Stress Cause a Stroke?
Stress triggers a cascade of physiological responses that begin in the brain and quickly affect the entire body. When an individual perceives a threat—whether it’s physical, emotional, or psychological, the hypothalamus activates the autonomic nervous system.
This in turn releases stress hormones, primarily cortisol and adrenaline, which prepare the body for a “fight or flight” response. While this reaction is protective in short bursts, chronic activation can lead to vascular inflammation, endothelial dysfunction, and elevated blood pressure, all of which are recognized contributors to stroke.
In particular, long-term stress can alter platelet function, increase the risk of clot formation, and accelerate arterial plaque buildup—all of which create conditions ripe for ischemic stroke, the most common type of stroke.
What Happens in the Body Under Stress?
On a molecular level, stress alters the balance of neurotransmitters and inflammatory markers. Cortisol, when persistently elevated, compromises the elasticity and integrity of blood vessels.
Adrenaline, while helpful in momentary threats, increases heart rate and constricts blood vessels, leading to sustained hypertension. These effects collectively burden the cardiovascular system, particularly the delicate cerebral arteries, which are more vulnerable to pressure-induced rupture or blockage.
Stress also increases insulin resistance and negatively affects lipid metabolism, which can indirectly increase stroke risk by promoting atherosclerosis.
What Are The Difference between Chronic Stress And Acute Stress
It’s important to differentiate between chronic and acute stress when evaluating stroke risk.
Chronic stress, which may result from long-term caregiving, financial instability, or unresolved trauma, leads to prolonged physiological strain. This type of stress contributes to sustained high blood pressure, poor lifestyle habits like overeating and smoking, and inflammation—all of which are long-term stroke risk factors.
On the other hand, acute emotional stress, such as receiving bad news or experiencing a sudden loss, can also lead to what is sometimes referred to as “stress cardiomyopathy” or even trigger a hemorrhagic stroke due to a sudden spike in blood pressure.
Both types of stress affect the cerebrovascular system but operate on different timeframes and mechanisms.
What Types of Stroke Are Linked to Stress?
Although stroke can occur for many reasons, stress is more commonly associated with ischemic strokes, where a blood clot obstructs the flow of blood to the brain.
This connection exists because stress can promote hypercoagulability, or an increased tendency for blood to clot. However, hemorrhagic strokes—caused by the rupture of a weakened blood vessel—can also result from acute emotional episodes, especially in individuals with untreated or poorly managed hypertension.
In some cases, high-stress events lead to what are known as transient ischemic attacks (TIAs), or mini-strokes, which serve as warning signs of a more serious event to come.
What Are the Three Main Causes of Stroke?
To fully appreciate how stress plays a role in stroke, it’s essential to understand the three foundational causes.
- First is hypertension, the most significant modifiable risk factor for stroke worldwide, often exacerbated by prolonged psychological stress.
- Second is atherosclerosis, which refers to the narrowing of arteries due to plaque buildup—something indirectly accelerated by chronic stress through unhealthy lifestyle habits and inflammation.
- Third is cardiac arrhythmias, such as atrial fibrillation, which can be triggered or worsened by anxiety and panic episodes, thus increasing the risk of embolic stroke.
All three causes can be either directly or indirectly influenced by the body’s response to stress.
Can Emotional Stress Cause a Stroke?
Emotional stress can be just as harmful as physical stress when it comes to the risk of stroke. Sudden grief, panic attacks, intense anger, or even moments of extreme joy can activate the sympathetic nervous system in a way that overwhelms the heart and blood vessels.
This phenomenon has been observed in what is known as Takotsubo cardiomyopathy, or broken heart syndrome, a temporary condition where the heart muscle weakens due to an emotional shock.
While often reversible, such episodes demonstrate how powerful emotional triggers can have somatic consequences, including increased risk for stroke through abrupt changes in blood pressure and vascular tone.
Can Stress Cause a Stroke in Young Adults?
Young adults, particularly those between the ages of 25 and 45, are not immune to the effects of stress. In fact, the combination of chronic work pressure, sleep deprivation, poor diet, and anxiety can make this age group particularly vulnerable.
While congenital heart conditions and lifestyle choices play a role, it’s increasingly recognized that psychological stress contributes to early-onset strokes. In many cases, these strokes are ischemic and occur in individuals who don’t exhibit traditional risk markers, suggesting that stress alone, through its effects on blood pressure and vascular inflammation, may be a silent but significant factor.
Can Stress Cause a Stroke in the Elderly?
Elderly individuals are especially susceptible to stress-induced strokes due to the cumulative effects of aging, comorbidities, and vascular fragility. Emotional stress in older adults—such as bereavement, isolation, or fear—can precipitate strokes by triggering blood pressure spikes or cardiac arrhythmias.
Additionally, this demographic often has underlying conditions like atrial fibrillation or carotid artery disease that amplify stroke risk when stress is introduced into the equation. Because their vascular systems are less resilient, the elderly require targeted interventions to reduce both psychological stress and medical risk factors.
Stroke Symptoms in Males and Females
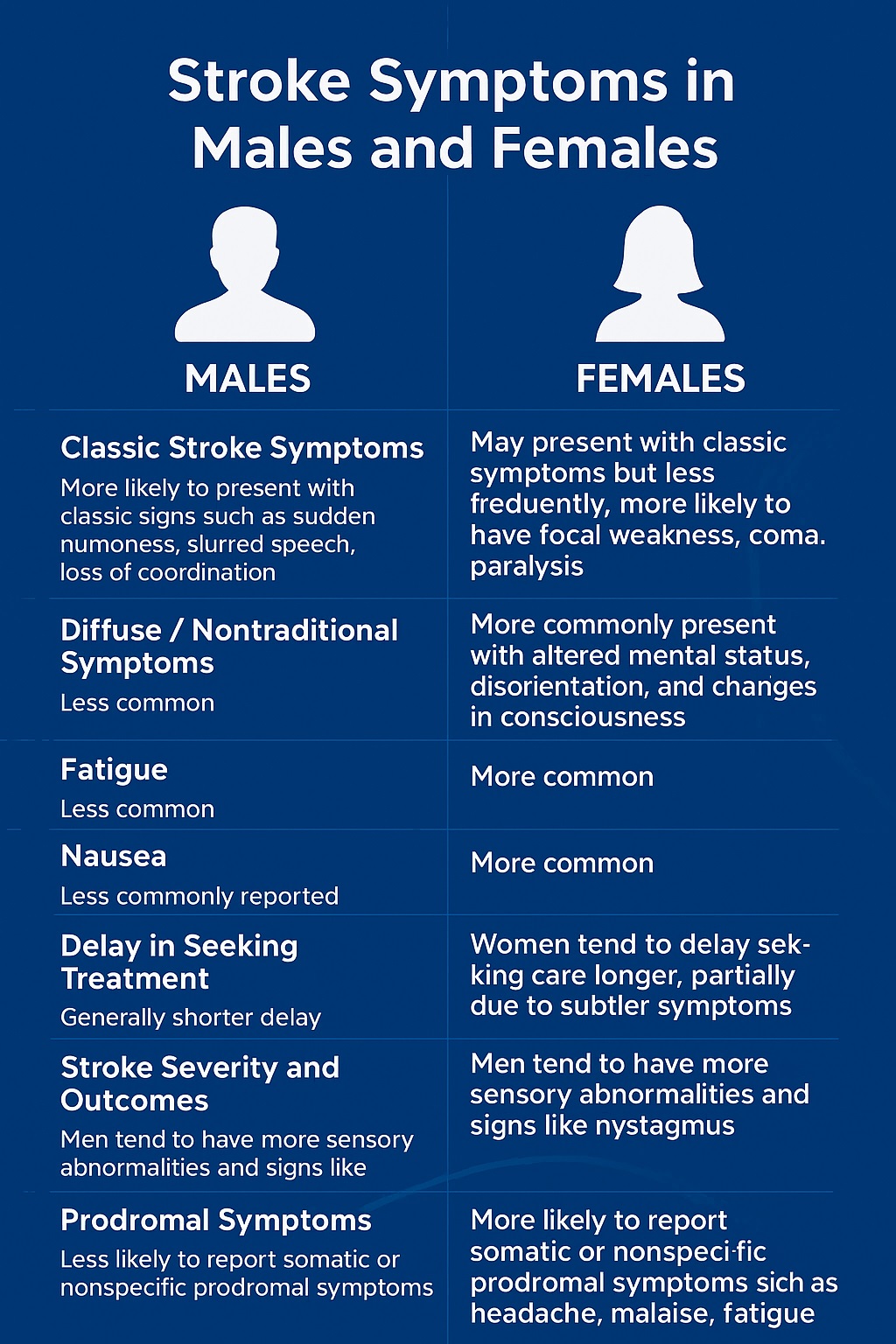
| Symptom / Feature |
Males |
Females |
| Classic Stroke Symptoms |
More likely to present with classic signs such as sudden numbness, slurred speech, loss of coordination, paresthesia, ataxia, double vision, nystagmus, sensory abnormalities |
May present with classic symptoms but less frequently; more likely to have focal weakness, coma, paralysis, aphasia, swallowing problems, urinary incontinence |
| Diffuse / Nontraditional Symptoms |
Less common |
More commonly present with diffuse or nontraditional symptoms such as generalized weakness, fatigue, disorientation, mental status changes, headache, face/limb pain, nausea, change in behavior, difficulty understanding, malaise, hiccups, shortness of breath, fever |
| Mental Status |
Less likely to show altered mental status |
More likely to present with altered mental status, disorientation, and changes in consciousness |
| Fatigue |
Less common |
More common |
| Nausea |
Less common |
More common |
| Hiccups |
Less commonly reported |
Reported more frequently |
| Delay in Seeking Treatment |
Generally shorter delay |
Women tend to delay seeking care longer, partially due to subtler symptoms |
| Stroke Severity and Outcomes |
Men tend to have more sensory abnormalities and signs like nystagmus |
Women tend to have higher mortality rates and worse outcomes, partly due to delayed treatment and older age at stroke onset |
| Prodromal Symptoms |
Less likely to report somatic or nonspecific prodromal symptoms |
More likely to report somatic prodromal symptoms such as headache, malaise, fatigue |
How to Reduce Stress and Avoid a Stroke
Preventing stroke in a high-stress world requires an integrative approach. Stress reduction is not just about relaxation; it’s about recalibrating the body’s response to pressure. Meditation, cognitive behavioral therapy, exercise, and even guided breathing techniques can reduce cortisol levels and improve vascular function. Additionally, improving sleep quality, limiting caffeine and alcohol, and nurturing social connections can mitigate the effects of stress over time. Long-term stroke prevention hinges not only on physical health but also on psychological resilience and emotional regulation.
What to Do to Avoid a Stroke?
To effectively reduce stroke risk, individuals must address both modifiable risk factors and lifestyle stressors. Monitoring and controlling blood pressure, managing cholesterol levels, and avoiding smoking are foundational.
Beyond that, maintaining a healthy weight, adopting a Mediterranean-style diet, and ensuring regular physical activity are critical. Mental health should not be sidelined in this equation.
Recognizing signs of burnout, anxiety, or depression and seeking appropriate treatment can be as lifesaving as managing blood sugar or reducing salt intake. The brain and the heart are in constant conversation, and both are heavily influenced by stress.
What Exercises Prevent Strokes?
- Aerobic Exercises: Walking, swimming, cycling, jogging
- Resistance Training: Weight lifting, bodyweight exercises
- Mind-Body Practices: Yoga, tai chi
Exercise recommendations suggest aiming for 150–300 minutes of moderate aerobic activity or 75–150 minutes of vigorous aerobic activity weekly, combined with resistance training 2–3 times per week. Even brief daily movement sessions can significantly lower stroke risk, especially for individuals prone to stress or with a family history of cardiovascular disease.
Frequently Asked Questions
What happens 1 month before a stroke?
There may be warning signs such as sudden weakness or numbness on one side of the body, trouble speaking or understanding speech, vision problems, dizziness, loss of balance or coordination, severe unexplained headaches, or transient ischemic attacks (TIAs or mini-strokes) that last minutes to hours and resolve.
These symptoms can occur shortly before a full stroke and should prompt immediate medical evaluation.
How do you know a stroke is coming?
You may notice sudden symptoms like facial drooping, arm weakness, slurred speech, confusion, vision loss, dizziness, or severe headache. TIAs or mini-strokes are important warning signs. Using the FAST acronym helps identify stroke signs quickly:
- Face drooping
- Arm weakness
- Speech difficulty
- Time to call for help
How to avoid paralysis?
Early treatment is critical to minimize brain damage and paralysis. After a stroke, rehabilitation exercises including passive and active movements, mental practice, electrical stimulation, acupuncture, and mirror therapy can help regain mobility by promoting neuroplasticity and rewiring the brain-muscle connection. Consistency and repetition in therapy are key to recovery.
What drinks prevent strokes?
While no single drink can prevent a stroke, overall hydration is important. Choosing healthy beverages like water and limiting sugary or alcoholic drinks supports overall cardiovascular health and helps reduce stroke risk.
What is first aid for stroke?
- Call emergency services immediately (911 or local emergency number).
- Check for stroke signs using FAST:
- Face drooping
- Arm weakness
- Speech difficulty
- Time to call for help
- Help the person lie down comfortably, preferably on their side with their head slightly elevated.
- Keep their airway clear; if unconscious, place them in the recovery position to prevent choking.
- Do not give food, drink, or medication.
- Stay calm, reassure them, and monitor breathing and consciousness until help arrives.
Can stress cause a heart attack?
Yes, stress can contribute to heart attacks by increasing blood pressure, causing inflammation, and leading to unhealthy behaviors that raise cardiovascular risk. Stress affects the heart and blood vessels, increasing the likelihood of heart attacks.
Can stress cause a mini stroke?
Yes, stress can increase the risk of transient ischemic attacks (TIAs or mini-strokes) by affecting blood pressure, circulation, and inflammation, which can temporarily block blood flow to the brain.