A nebulizer is a medical device that converts liquid medication into a fine mist, allowing it to be inhaled directly into the lungs. This method delivers treatment faster and more efficiently, especially for individuals who have difficulty using inhalers. According to the
American College of Allergy, Asthma, and Immunology (ACAAI), nebulizers are often recommended for treating respiratory illnesses such as asthma, bronchitis, and chronic obstructive pulmonary disease (COPD), all of which may include chronic coughing as a symptom.
The Centers for Disease Control and Prevention (CDC) notes that approximately 25 million people in the U.S. have asthma, and nearly 50% of them report experiencing at least one asthma attack each year. Nebulizers play a key role in managing these attacks by opening the airways, reducing inflammation, and easing symptoms such as coughing, wheezing, and shortness of breath.
For children and elderly patients who struggle with inhaler coordination, nebulizers are a safer and more effective alternative. The National Heart, Lung, and Blood Institute (NHLBI) highlights that nebulizer treatment is particularly useful for delivering high doses of medication during acute respiratory distress episodes, especially when rapid relief is necessary.
By moisturizing the airways, delivering bronchodilators, and supporting medication absorption deep into the lungs, nebulizers provide targeted relief. This helps in breaking the cycle of persistent coughing caused by airway irritation, mucus buildup, or bronchospasm. When used as prescribed, nebulizer therapy can significantly reduce the duration and severity of coughing episodes tied to respiratory conditions.
What Types of Coughs Can a Nebulizer Treat?
Nebulizer for Wet or Productive Cough
A productive cough involves mucus or phlegm. Nebulizers help loosen and thin this mucus, making it easier to expel. Saline solutions or bronchodilators such as albuterol are often used to open airways and facilitate mucus drainage. This type of treatment supports better airflow and reduces chest tightness.
Nebulizer for Dry Cough
Dry coughs are often caused by irritation or inflammation in the airways. Nebulized saline or anti-inflammatory medications like budesonide can soothe the airways and reduce coughing episodes. Moisturizing the respiratory tract can decrease throat irritation and suppress persistent dry cough.
Nebulizer for Asthma-Related or Allergic Cough
For asthma or allergy-induced coughs, a nebulizer delivers corticosteroids or bronchodilators to reduce airway inflammation and ease breathing. This is especially helpful during flare-ups or allergy seasons. The targeted mist relaxes the bronchial muscles and prevents airway constriction.
What to Put in a Nebulizer for Cough Relief
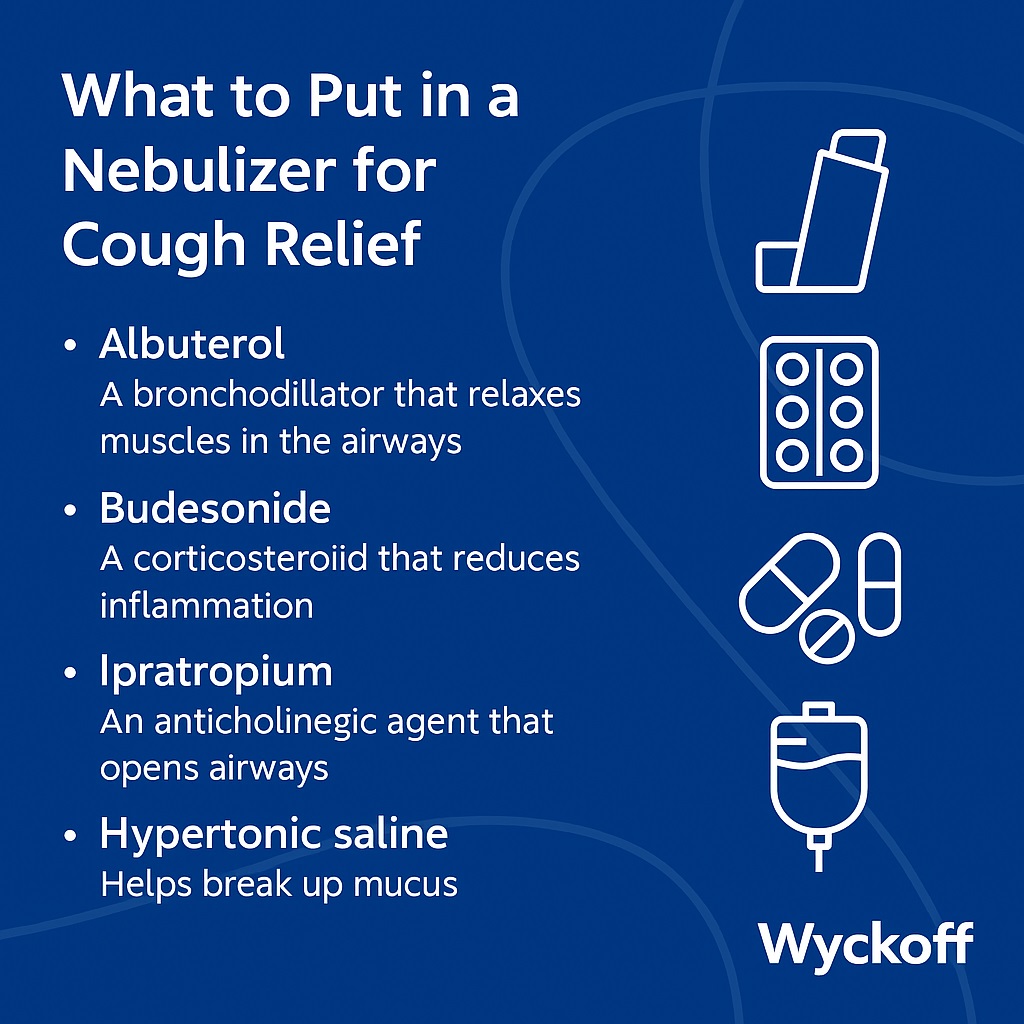
The effectiveness of nebulizer treatment depends largely on the medication used. Common nebulizer medications for cough include:
- Albuterol: A bronchodilator that relaxes muscles in the airways.
- Budesonide: A corticosteroid that reduces inflammation.
- Ipratropium: An anticholinergic agent that opens airways.
- Hypertonic saline: Helps break up mucus.
Note: These medications should only be used under the guidance of a healthcare provider. Over-the-counter or prescription options must be selected based on the type of cough and overall health status.
Can You Use a Nebulizer at Home?
Yes, nebulizers can be safely used at home with proper instructions. A home nebulizer kit includes a compressor, tubing, mouthpiece or mask, and medication cup. Treatment sessions usually last between 10 to 20 minutes.
To ensure effective therapy, it’s essential to maintain good hygiene: clean the parts after each use, store them in a dust-free area, and use sterile medication solutions.
Is It Safe to Use a Nebulizer at Night or During a Chest Infection?
Using a nebulizer at night can be beneficial for people with nighttime coughing fits or asthma symptoms. However, if you have a fever or signs of a severe infection, always consult a doctor before using the device.
During chest infections, doctors may prescribe antibiotics or steroids via nebulizer, especially when mucus buildup or inflammation is severe. Avoid using a nebulizer without medical supervision if your condition worsens.
Can Babies or Children Use a Nebulizer?
Yes, nebulizers are commonly used for infants and young children, especially those with RSV, asthma, or persistent coughs. A pediatric nebulizer typically includes a smaller mask and lower medication doses.
It’s crucial to follow the pediatrician’s prescription to ensure safety and effectiveness.
What is the difference between Steam Inhalation and Nebulization
While both methods involve inhaling moisture, steam delivers general humidity to the upper airways, whereas nebulization introduces medicated mist directly into the lungs. Steam is good for soothing throat irritation and nasal congestion. In contrast, nebulizers are better for lower respiratory issues like asthma, bronchitis, and chronic obstructive pulmonary disease (COPD).
What is the difference between Nebulizer and Inhaler
Inhalers are portable and fast-acting but require proper technique, which may be difficult for some patients, especially young children or the elderly. Nebulizers are easier to use for people with limited coordination and are ideal during acute flare-ups. The choice depends on the condition being treated and the patient’s ability to use the device effectively.
What Are the Side Effects of Using a Nebulizer?
Common side effects of using a nebulizer may include:
-
- Jitteriness
- Rapid heartbeat
- Nausea
- Throat irritation
- Headaches
These effects are generally caused by the medication used rather than the nebulizer device itself. Serious side effects that require immediate medical attention include:
-
- Chest pain
- Swelling
- Difficulty breathing
How to Clean and Maintain Your Nebulizer
- After each treatment session, disconnect and rinse all nebulizer parts except for the tubing.
- Wash the medication cup, mouthpiece, or mask with warm water and mild soap.
- Rinse thoroughly under clean running water to remove soap residue.
- Shake off excess water and let all parts air-dry on a clean towel.
- Once a week, disinfect the nebulizer parts by soaking them in a vinegar-water solution (1 part vinegar to 3 parts water) for 20 minutes.
- Rinse again with clean water and allow everything to dry completely before reassembling.
- Store the nebulizer in a clean, dry, and dust-free environment.
Can a Nebulizer Be Used for Cold and Flu?
While nebulizers are not typically used for mild colds, they can help manage symptoms in patients with underlying respiratory conditions. If a cold leads to wheezing or chest congestion, a nebulizer may provide relief.
However, for general cold symptoms like runny nose or sore throat, traditional remedies such as rest, fluids, and over-the-counter medications are usually sufficient.
What’s the Best Medicine for Nebulizer Cough Relief?
The best medicine for nebulizer cough relief is often albuterol. It is a fast-acting bronchodilator that helps open the airways, especially effective for wheezing, asthma-related coughs, and bronchospasms. If inflammation is the primary cause, budesonide—a corticosteroid—is commonly prescribed to reduce swelling in the airways and suppress persistent coughing.
For coughs with thick mucus or congestion, hypertonic saline works by thinning the mucus and making it easier to expel. Ipratropium, an anticholinergic medication, is another option for relieving airway constriction.
When to See a Doctor for a Cough
Seek medical attention if your cough lasts more than three weeks, worsens over time, produces blood, or comes with weight loss, fever, or difficulty breathing. A persistent or severe cough may signal a more serious condition that requires targeted treatment.
If you are in Brooklyn and need expert care, Wyckoff Heights Medical Center provides comprehensive respiratory evaluations and treatments. Their experienced pulmonologists and internal medicine specialists are equipped to manage both acute and chronic cough conditions with personalized care plans.
Nebulizer Use for COPD, Asthma, and Bronchitis
Nebulizers play a critical role in managing chronic respiratory diseases. For COPD and asthma, they deliver long-acting bronchodilators or corticosteroids to maintain airway function. In bronchitis, they help reduce inflammation and loosen mucus. Consistent use, as prescribed, improves lung capacity and reduces symptom flare-ups.
FAQs About Nebulizers for Cough
What If You’re Still Coughing After Using a Nebulizer?
Continued coughing after nebulizer treatment can occur due to incorrect medication, improper device use, or an untreated underlying condition. If symptoms persist, it’s essential to revisit your doctor. Sometimes, a different treatment or a combination of therapies—including oral medications or antibiotics—may be necessary to resolve the issue fully.
Does a Nebulizer Stop Coughing Immediately?
Yes, a nebulizer can help stop coughing quickly, especially in respiratory conditions like asthma, bronchitis, COPD, and RSV. It provides fast relief by delivering medication directly into the lungs, where it works to relax the airway muscles, reduce inflammation, and thin mucus.
Symptoms such as wheezing, chest tightness, persistent dry or wet cough, and shortness of breath often respond well to nebulizer treatment. Relief typically begins within minutes when using medications like albuterol, although effectiveness may vary based on the cause and severity of the cough.
Can You Use a Nebulizer with Just Water or Saline?
Yes, but only sterile saline or sterile water should be used—not tap or distilled water. Use 0.9% normal saline or sterile water labeled for inhalation. These hydrate airways, loosen mucus, and ease dry cough. Avoid non-sterile water types, which can irritate or infect the lungs.
Can You Use a Nebulizer Without Medication?
Using a nebulizer with just saline solution can help hydrate airways and reduce coughing in cases of mild irritation or dry air exposure. However, it should not be used as a substitute for prescribed medications in treating respiratory diseases. Avoid using essential oils or other substances not approved for inhalation, as they can damage the lungs.
What’s the Best Time of Day to Use a Nebulizer?
The best time of day to use a nebulizer is morning and evening, because symptoms like wheezing and coughing tend to worsen during these times. Using it then helps open the airways, improves breathing, and ensures medication works when it’s most needed.
Can You Sleep Right After a Nebulizer Treatment?
Yes, you can sleep after using a nebulizer, especially if it relieves nighttime coughing. It’s best to use it before bed to prevent overnight symptoms. Morning and mid-afternoon sessions are also effective for managing breathing and keeping symptoms under control throughout the day.
Can You Travel with a Nebulizer?
Yes, portable and battery-operated nebulizers are available. Carry your prescription and extra medication when traveling.